
Popular topics

-
References
Bhattacharjee S and Lukiw WJ (2013). Alzheimer's disease and the microbiome. Front Cell Neurosci 7,153.
Bondareff W et al. (1987). Neuronal degeneration in locus ceruleus and cortical correlates of Alzheimer disease. Alzheimer Dis Assoc Disord 1, 256-262.
Bowen DM et al. (1976). Neurotransmitter-related enzymes and indices of hypoxia in senile dementia and other abiotrophies. Brain 99, 459-496.
Chételat G et al. (2013). Amyloid imaging in cognitively normal individuals, at-risk populations and preclinical Alzheimer's disease. NeuroImage Clin 2, 356-365.
Chiroma SM et al. (2018). Inflammation in Alzheimer’s disease: A friend or foe? Biomedical Research and Therapy 5, 2,552-2,564.
Clavaguera F et al. (2009). Transmission and spreading of tauopathy in transgenic mouse brain. Nat Cell Biol 11, 909-913.
Davies, P and Maloney, AJ (1976). Selective loss of central cholinergic neurons in Alzheimer’s disease. Lancet 2, 1,403.
Deardorff WJ and Grossberg GT (2017). Targeting neuroinflammation in Alzheimer's disease: evidence for NSAIDs and novel therapeutics. Expert Rev Neurother 17,17-32.
Doody RS et al. (2013). A Phase 3 Trial of Semagacestat for treatment of Alzheimer's disease. N Engl J Med 369, 341-350.
Du X et al. (2018). Alzheimer's disease hypothesis and related therapies. Transl neurodegener 7, 2.
Ferreira-Vieira et al. (2016). Alzheimer's disease: targeting the cholinergic system. Curr Neuropharmacol 14, 101-115.
Frost B et al. (2009). Propagation of tau misfolding from the outside to the inside of a cell. J Biol Chem 284,12,845-12,852.
Goedert, M and Spillantini MG (2017). Propagation of Tau aggregates. Mol Brain 10, 18.
Hardy JA and Higgins GA (1992). Alzheimer's disease: the amyloid cascade hypothesis. Science 256,184-185.
Hickman SE et al. (2008). Microglial dysfunction and defective beta-amyloid clearance pathways in aging Alzheimer's disease mice. J Neurosci 28, 8,354-8,360.
Hirbec HE et al. (2017). Microglia responses in acute and chronic neurological diseases: What microglia-specific transcriptomic studies taught (and did not teach) us. Front Aging Neurosci 9, 227.
Liu P et al. (2019). History and progress of hypotheses and clinical trials for Alzheimer’s disease. Signal Transduct Target Ther 4, 29.
Marizzoni M et al. (2020) Short-chain fatty acids and lipopolysaccharide as mediators between gut dysbiosis and amyloid pathology in Alzheimer’s disease. J Alzheimers Dis 78, 683-697.
Ozben T and Ozben S (2019). Neuro-inflammation and anti-inflammatory treatment options for Alzheimer's disease. Clin Biochem 72, 87-89.
Price JL et al. (2009). Neuropathology of nondemented aging: presumptive evidence for preclinical Alzheimer disease. Neurobiol Aging 30,1,026-1,036.
Prince M et al. (2015). The Global impact of dementia: An analysis of prevalence, incidence, cost and trends, World Alzheimer Report, Alzheimer’s Disease International (ADI), London. https://www.alzint.org/resource/world-alzheimer-report-2015/. Accessed 05/13/21.
Raina P (2008). Effectiveness of cholinesterase inhibitors and memantine for treating dementia: evidence review for a clinical practice guideline. Ann Intern Med 148 5, 379.
Rogers J et al. (1988). Expression of immune system-associated antigens by cells of the human central nervous system: relationship to the pathology of Alzheimer's disease. Neurobiol Aging 9, 339-349.
Ross JA et al. (2015). Locus coeruleus, norepinephrine and Abeta peptides in Alzheimer's disease. Neurobiol Stress 2, 73-84.
Sameem B et al. (2017). A review on tacrine-based scaffolds as multi-target drugs (MTDLs) for Alzheimer's disease. Eur J Med Chem 128, 332-345.
Sanders L (2021). FDA approved a new Alzheimer’s drug despite controversy over whether it works. Science News. Accessed 06/17/2021
Sanz-Blasco S et al. (2018). Is it all said for NSAIDs in Alzheimer's disease? Role of mitochondrial calcium uptake. Curr Alzheimer Res 15, 504-510.
Siemersa ER et al. (2016). Phase 3 solanezumab trials: Secondary outcomes in mild Alzheimer's disease patients. Alzheimers Dement 12,110-120.
Snowdon DA (1997). Aging and Alzheimer’s Disease: Lessons from the Nun Study. Gerontologist 37,150-156.
Sureda A et al. (2019). Oral microbiota and Alzheimer’s disease: Do all roads lead to Rome? Pharmacol Res 151, 104,582.
Vandenberghe R et al. (2016). Bapineuzumab for mild to moderate Alzheimer's disease in two global, randomized, phase 3 trials. Alzheimers Res Ther 8, 18.
Wang J et al. (2017). A systemic view of Alzheimer disease — insights from a myloid-beta metabolism beyond the brain. Nat Rev Neurol 13, 612-623.
Whitehouse PJ et al. (1981). Alzheimer disease: evidence for selective loss of cholinergic neurons in the nucleus basalis. Ann Neurol 10, 122-126.
Zarow C et al. (2003). Neuronal loss is greater in the locus coeruleus than nucleus basalis and substantia nigra in Alzheimer and Parkinson diseases. Arch Neurol 60, 337-341.
What Causes Alzheimer’s Disease?
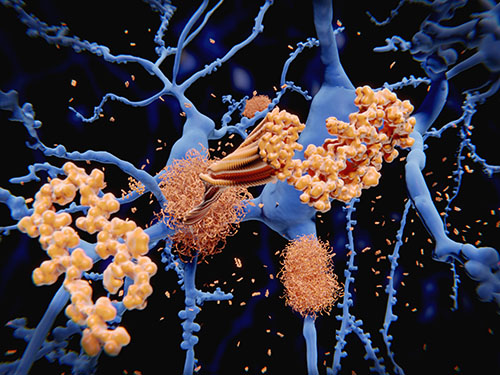
Alzheimer's disease is a neurodegenerative disorder characterized by progressive memory loss, cognitive function impairment, and neuropsychiatric symptoms, such as apathy, depression, and sometimes even hallucinations. This disease is the most common type of dementia, affecting around 50 million people worldwide (Prince et al. 2015). The main pathophysiological features include brain atrophy and neuronal loss due to tau tangles, amyloid-β plaques, and neuroinflammation.
Alzheimer's disease is a multifactorial disorder with genetic, environmental, and aging risk factors. Over the years, different hypotheses have been put forward to explain Alzheimer's disease pathophysiology, but the ultimate disease etiology is still not clear. In this blog, we summarize some of the various hypotheses that have been proposed over the years and the more recent idea that gut microbiota may play a role in disease development.
The Amyloid-β Cascade Hypothesis
One of the oldest hypotheses as to the cause of Alzheimer's disease is based on the discovery of plaques in the brains of patients with early-onset dementia. These depositions of amyloid-β were believed to initiate a cascade that leads to the neuronal loss, neurofibrillary tangles, vascular damage, dementia, and cognitive impairment that are characteristic of Alzheimer's disease (Hardy and Higgins 1992).
While amyloid-β may provide a strategy for the diagnosis of Alzheimer’s, as a pathological feature, there is a lack of evidence to support that amyloid-β is the primary trigger of Alzheimer's disease and this hypothesis has fallen out of favor. Autopsies and imaging studies did not support this proposed relationship between amyloid-β aggregations and clinical symptoms in Alzheimer's disease patients (Chételat et al. 2013, Price et al. 2009, Snowdon 1997). Moreover, anti-amyloid‑β therapeutic trials, that inhibit amyloid-β aggregation, have failed to demonstrate curative results: some trials targeted amyloid-β (Siemersa et al. 2016, Vandenberghe et al. 2016) and others γ-secretase (Doody et al. 2013), but neither showed an improvement in Alzheimer's disease patients. Additionally, while a recent FDA approved drug, aducanumab, demonstrated a reduction in amyloid-β plaques in the brain, it’s approval was controversial due to an earlier trial failing to show evidence that it slowed Alzheimer’s progression and the drug may have only offer marginal benefits (Sanders 2021).
The Tau Hypothesis
Intracellular “tau tangles” are an important pathological feature of Alzheimer’s disease. These tangles are formed from hyperphosphorylated tau proteins and "The Tau Propagation Hypothesis" suggests that these neurofibrillary tangles could spread through cells in the same way as prions (Clavaguera et al. 2009, Frost et al. 2009). Tau tangles usually appear in discrete areas of the brain before spreading further as an endopathogen (Clavaguera et al. 2009). This misfolded Tau protein can induce the same aberrant conformation to other Tau proteins when engulfed into healthy cells, amplifying the cascade (Goedert and Spillantini 2017).
While this mechanism does correlate better than amyloid-β pathology with the clinical features of this dementia, there is only limited evidence to support the idea that tauopathy triggers Alzheimer's disease. Similarly to amyloid-β, most clinical trials aimed at blocking tau aggregation have also failed (Du et al. 2018). There are still a number of tau-directed therapies in clinical trials, so their overall effectiveness remains to be determined (Liu et al. 2019).
The Inflammation Hypothesis
Since 1988, different studies have suggested a relationship between the immune system and Alzheimer's disease (Rogers et al. 1988). This hypothesis suggests that the enhanced production of pro-inflammatory cytokines exacerbates both amyloid‑β and tau pathologies. However, no factor has been discovered to be responsible for initiating local inflammation and it is unclear whether inflammation leads to Alzheimer's disease, or if inflammation results from pathological features of Alzheimer's disease (Chiroma et al. 2018).
An important argument against "The Inflammation Hypothesis" as the trigger of Alzheimer's disease is that nonsteroid anti-inflammatory drugs (NSAIDs), like naproxen and celecoxib, have not yielded beneficial effects (Deardorff and Grossberg 2017, Ozben and Ozben 2019, Sanz-Blasco et al. 2018). If inflammation was key to the development of Alzheimer’s disease, then you would anticipate the use of NSAIDs to offer protection by delaying the onset or occurrence of the condition.
The complexity of the immune response in Alzheimer's disease depends on the diverse functions of glial cells. Among them, microglia (brain-specific macrophages in the central nervous system (CNS)) vary in a wide range of phenotypes (Hirbec et al. 2017), making them very difficult to target for neuronal homeostasis recovery. There is still much to be discovered about the regulation of neuroinflammation and microglial activation, especially as early microglial activation in Alzheimer’s disease supports amyloid-β clearance and is neuroprotective. It is later in the disease that amyloid-β aggregation and proinflammatory cytokines lead to a reduction in amyloid-β clearance and neurodegeneration (Hickman et al. 2008).
The Cholinergic Hypothesis
“The Cholinergic Hypothesis” was the first hypothesis to change the way we think about Alzheimer’s disease: instead of describing Alzheimer’s disease neuropathology, it uses the contemporary idea of synaptic neurotransmission (Bowen et al. 1976, Davies and Maloney 1976, Whitehouse et al. 1981).This hypothesis was proposed by Davies and Maloney in 1976 after studying neurotransmitters in the brains of Alzheimer’s patients (Davies and Maloney 1976). They observed a reduction of choline acetyltransferase in key brain regions and a reduction in the concentration of the neurotransmitter acetylcholine at synapses. They postulated that a progressive decrease of acetylcholine, and loss of cholinergic neurons, contribute significantly to the cognitive decline observed in Alzheimer's disease patients. This hypothesis centers on the loss of limbic and neocortical cholinergic innervation, which correlates with Alzheimer’s disease signs, such as release of amyloid-β, hyperphosphorylation of tau, cognitive dysfunction, and disease progression (Ferreira-Vieira et al. 2016). However, the exact mechanism by which the cholinergic impairment affects cognition, and behavior, is unknown.
While cholinesterase inhibitors can improve the cognitive symptoms of dementia (Raina 2008), they have no significant effect on the occurrence or progression of Alzheimer’s disease, with too many side effects and not enough beneficial results (Sameem et al. 2017). Additionally, the cholinergic loss produced in Alzheimer's disease depends directly on the noradrenergic deficit (Zarow et al. 2003).
The Noradrenergic Hypothesis
In 1987, “The Noradrenergic Hypothesis” was first related to Alzheimer's disease (Bondareff et al.1987). The locus coeruleus represents the main source of noradrenergic innervation to the CNS and its degeneration is a crucial early event in the pathogenesis of Alzheimer’s disease. The degeneration of the locus coeruleus exacerbates inflammatory responses that provoke the release of cytotoxins and induce amyloid‑β accumulation (Ross et al. 2015).
This hypothesis suggests that recovering noradrenaline levels in the CNS will prevent the neurodegeneration and cognitive decline of Alzheimer's disease and the theory is complementary to the amyloid-β cascade, tau, inflammation, and cholinergic Alzheimer's disease hypotheses.
However, while targeting the noradrenergic dysfunction in Alzheimer’s patients is a tantalizing concept, to develop therapies, the role of the locus coeruleus-noradrenaline system needs to be better understood at different stages of the progression of Alzheimer's disease, and warrants further research.
The Emerging Role of the Gut
Recent studies have considered Alzheimer's disease to be a disease not only restricted to the CNS but also related to the gut microbiome. The arguments are based on the communication between gut microbiota and the brain through the immune system, the endocrine pathway, and the vagus nerve and bacteria-derived metabolites (Bhattacharjee and Lukiw 2013, Du et al. 2018). A study in 2020 confirmed the correlation between reduced gut microbiota composition and amyloidosis through inflammatory mediators in the blood (Marizzoni 2020).
In this hypothesis, proteins associated with inflammation and synthesized by specific intestinal bacteria, such as lipopolysaccharides and short-chain fatty acids (acetate and valerate), are found in the blood of Alzheimer's disease patients and correlate with large amyloid plaque deposition in the brain. Conversely, the researchers found that high levels of another short-chain fatty acid, butyrate, were associated with a reduction in amyloid pathology.
It is suggested that inflammation in the blood could be impairing the regulation between the immune system and the brain (Marizzoni 2020). This new perspective broadens the possibilities to understand Alzheimer's disease and opens up avenues into new treatment options, involving manipulating gut microbiota to prevent Alzheimer’s disease. However, this hypothesis is still in its infancy, and more research is needed before studying drugs aiming at the gut's microbiome to cure Alzheimer's disease.
Developing Theories
New hypotheses are trying to understand the physiopathology of Alzheimer's disease. Systemic abnormalities in Alzheimer's disease are also being studied, such as disorders of systemic immunity, cardiovascular diseases, hepatic dysfunctions, metabolic disorders, blood defects, respiratory and sleep disorders, renal dysfunctions, microbiota disturbance and infection, systemic inflammation (Wang et al. 2017), and oral microbiota (Sureda et al. 2019).
In conclusion, none of the hypotheses alone can so far explain the neuronal impairment in Alzheimer's disease thoroughly. Although new perspectives may be necessary, it is possible that one of the proposed hypotheses could relay the trigger of Alzheimer's disease. Understanding and controlling the neuroimmunology in these patients could be vital in preventing or decelerating the disease. Therefore, to completely comprehend Alzheimer's disease pathophysiology, more investigations need to be carried out at different stages of the progression of the disease to identify new therapeutic targets.
Interested in the Role of Microglia?
Find out about how microglia may drive neuroinflammation and Alzheimer’s disease in our micro-review.
References
Bhattacharjee S and Lukiw WJ (2013). Alzheimer's disease and the microbiome. Front Cell Neurosci 7,153.
Bondareff W et al. (1987). Neuronal degeneration in locus ceruleus and cortical correlates of Alzheimer disease. Alzheimer Dis Assoc Disord 1, 256-262.
Bowen DM et al. (1976). Neurotransmitter-related enzymes and indices of hypoxia in senile dementia and other abiotrophies. Brain 99, 459-496.
Chételat G et al. (2013). Amyloid imaging in cognitively normal individuals, at-risk populations and preclinical Alzheimer's disease. NeuroImage Clin 2, 356-365.
Chiroma SM et al. (2018). Inflammation in Alzheimer’s disease: A friend or foe? Biomedical Research and Therapy 5, 2,552-2,564.
Clavaguera F et al. (2009). Transmission and spreading of tauopathy in transgenic mouse brain. Nat Cell Biol 11, 909-913.
Davies, P and Maloney, AJ (1976). Selective loss of central cholinergic neurons in Alzheimer’s disease. Lancet 2, 1,403.
Deardorff WJ and Grossberg GT (2017). Targeting neuroinflammation in Alzheimer's disease: evidence for NSAIDs and novel therapeutics. Expert Rev Neurother 17,17-32.
Doody RS et al. (2013). A Phase 3 Trial of Semagacestat for treatment of Alzheimer's disease. N Engl J Med 369, 341-350.
Du X et al. (2018). Alzheimer's disease hypothesis and related therapies. Transl neurodegener 7, 2.
Ferreira-Vieira et al. (2016). Alzheimer's disease: targeting the cholinergic system. Curr Neuropharmacol 14, 101-115.
Frost B et al. (2009). Propagation of tau misfolding from the outside to the inside of a cell. J Biol Chem 284,12,845-12,852.
Goedert, M and Spillantini MG (2017). Propagation of Tau aggregates. Mol Brain 10, 18.
Hardy JA and Higgins GA (1992). Alzheimer's disease: the amyloid cascade hypothesis. Science 256,184-185.
Hickman SE et al. (2008). Microglial dysfunction and defective beta-amyloid clearance pathways in aging Alzheimer's disease mice. J Neurosci 28, 8,354-8,360.
Hirbec HE et al. (2017). Microglia responses in acute and chronic neurological diseases: What microglia-specific transcriptomic studies taught (and did not teach) us. Front Aging Neurosci 9, 227.
Liu P et al. (2019). History and progress of hypotheses and clinical trials for Alzheimer’s disease. Signal Transduct Target Ther 4, 29.
Marizzoni M et al. (2020) Short-chain fatty acids and lipopolysaccharide as mediators between gut dysbiosis and amyloid pathology in Alzheimer’s disease. J Alzheimers Dis 78, 683-697.
Ozben T and Ozben S (2019). Neuro-inflammation and anti-inflammatory treatment options for Alzheimer's disease. Clin Biochem 72, 87-89.
Price JL et al. (2009). Neuropathology of nondemented aging: presumptive evidence for preclinical Alzheimer disease. Neurobiol Aging 30,1,026-1,036.
Prince M et al. (2015). The Global impact of dementia: An analysis of prevalence, incidence, cost and trends, World Alzheimer Report, Alzheimer’s Disease International (ADI), London. https://www.alzint.org/resource/world-alzheimer-report-2015/. Accessed 05/13/21.
Raina P (2008). Effectiveness of cholinesterase inhibitors and memantine for treating dementia: evidence review for a clinical practice guideline. Ann Intern Med 148 5, 379.
Rogers J et al. (1988). Expression of immune system-associated antigens by cells of the human central nervous system: relationship to the pathology of Alzheimer's disease. Neurobiol Aging 9, 339-349.
Ross JA et al. (2015). Locus coeruleus, norepinephrine and Abeta peptides in Alzheimer's disease. Neurobiol Stress 2, 73-84.
Sameem B et al. (2017). A review on tacrine-based scaffolds as multi-target drugs (MTDLs) for Alzheimer's disease. Eur J Med Chem 128, 332-345.
Sanders L (2021). FDA approved a new Alzheimer’s drug despite controversy over whether it works. Science News. Accessed 06/17/2021
Sanz-Blasco S et al. (2018). Is it all said for NSAIDs in Alzheimer's disease? Role of mitochondrial calcium uptake. Curr Alzheimer Res 15, 504-510.
Siemersa ER et al. (2016). Phase 3 solanezumab trials: Secondary outcomes in mild Alzheimer's disease patients. Alzheimers Dement 12,110-120.
Snowdon DA (1997). Aging and Alzheimer’s Disease: Lessons from the Nun Study. Gerontologist 37,150-156.
Sureda A et al. (2019). Oral microbiota and Alzheimer’s disease: Do all roads lead to Rome? Pharmacol Res 151, 104,582.
Vandenberghe R et al. (2016). Bapineuzumab for mild to moderate Alzheimer's disease in two global, randomized, phase 3 trials. Alzheimers Res Ther 8, 18.
Wang J et al. (2017). A systemic view of Alzheimer disease — insights from a myloid-beta metabolism beyond the brain. Nat Rev Neurol 13, 612-623.
Whitehouse PJ et al. (1981). Alzheimer disease: evidence for selective loss of cholinergic neurons in the nucleus basalis. Ann Neurol 10, 122-126.
Zarow C et al. (2003). Neuronal loss is greater in the locus coeruleus than nucleus basalis and substantia nigra in Alzheimer and Parkinson diseases. Arch Neurol 60, 337-341.
You may also be interested in...

View more Neuroscience or Article blogs















