
Popular topics

-
References
ClinicalTrials.gov NCT04353128, Efficacy of melatonin in the prophylaxis of coronavirus infectious disease 2019 (COVID-19) among healthcare workers (The MeCOVID Study). (MeCOVID).
Estes C (2020). What is the cytokine storm and why is it so deadly for coronavirus patients? Forbes. Accessed on 04/28/2020
Goodman B (2020). Cytokine storms may be fueling some COVID deaths. WebMD Health News 17 April 2020. Accessed on 04/28/2020
Guo XJ and Thomas PG (2018). New fronts emerge in the influenza cytokine storm, Semin Immunopathol 39, 541–550.
NICE guideline NG51 (2017). Sepsis: recognition, diagnosis and early management. Available at: www.nice.org.uk/guidance/ng51/chapter/recommendations#risk-factors-for-sepsis. Accessed 04/28/2020
Rizzo P et al. (2020). COVID-19 in the heart and the lungs: could we “Notch” the inflammatory storm? Basic Res Cardiol 115, 31.
Tisoncik JR et al. (2012). Into the eye of the cytokine storm. Microbiol Mol Biol Rev 76, 16–32.
Wu D and Yang XO (2020). TH17 responses in cytokine storm of COVID-19: An emerging target of JAK2 inhibitor Fedratinib. J Microbiol Immunol Infect Epub ahead of print.Accessed 04/28/2020
Ye Q et al. (2020). The pathogenesis and treatment of the `cytokine storm' in COVID-19. J Infect Epub ahead of print. Accessed 04/28/2020
Zhang R et al. (2020). COVID-19: Melatonin as a potential adjuvant treatment, Life Sci 250: 117583.
Zhang W et al. (2020). The use of anti-inflammatory drugs in the treatment of people with severe coronavirus disease 2019 (COVID-19): The experience of clinical immunologists from China. Clin Immunol Epub ahead of print. Accessed 04/28/2020
Navigating the Deadly Cytokine Storm
It can be comforting to compare our immune system to an intruder alarm, ready to lockdown the premises and release angry guard dogs when a threat approaches. Most of the time, like home security, our immune systems work to our advantage. But what if a home intruder alarm was activated every time you came home from work, or failed to deactivate after an unwelcome visitor has been escorted away?
It isn’t uncommon for our immune system to betray us, launching a co-ordinated assault against a non-threatening substance such as dust or pollen. Healthy cells that we depend on for survival can be attacked by our immune systems, a destructive process known too well by those with autoimmune disorders.
Another common situation is for our immune system to launch an excessive, disproportionate response to a real infection. The immune system starts attacking everything in sight, including healthy tissues (Guo and Thomas 2018). This life-threatening condition involves a “cytokine storm”, and appears to be a significant cause of death among patients hospitalized with severe COVID-19 (Goodman 2020). Understanding the trajectory of the storm and how to subdue it could help clinicians prevent deaths.
Cytokine Storms: an Immune Over-Reaction
Viruses require host cells in order to divide and reproduce. Our immune system tries to prevent the infection then spreading to neighboring cells. Virus-infected cells send out distress signals, recruiting immune cells to destroy them (Estes 2020). Cytokines are an essential part of this process, helping maintain a suitable environment for the immune system to eliminate the threat. Some cytokines like IL-6 help build a fever, enabling a high temperature that ensures our immune system works efficiently (Wu and Yang 2020).
While an immune response is necessary for eliminating a virus, disproportionate inflammation can be destructive. Some patients experience an uncontrolled immune response, leading to more and more inflammation. In patients with COVID-19, cytotoxic immune cells recruited to the lungs should only kill infected cells; however, some continue to destroy everything in their path, including healthy cells (Estes 2020). This hyperactive immune response can lead to acute lung injury (ALI) and may progress to acute respiratory distress syndrome (ARDS), lung failure, and death (Ye et al. 2020). A cytokine storm – release of too many cytokines into the blood too quickly – appears to be central to development of ALI, ARDS, and life-threatening sepsis (blood poisoning).
The Path of a Cytokine Storm
Awareness of cytokine storms took off during the 1990s, during the H5N1 “bird flu” epidemic. Cytokine storms present as systemic inflammation, multiple organ failure, and high inflammatory parameters like TNF (Zhang W et al. 2020). Cytokine storms have been documented in several infectious diseases and rheumatic diseases, and can also result from tumor immunotherapy.
Studies of patients with severe sepsis have revealed that the cytokine storm follows a characteristic pattern as it develops (Figure 1). In the minutes to hours after infection, levels of the acute response cytokines TNF and IL-1β and the chemotactic cytokines IL-8 and MCP-1 are elevated. This is followed by an increase in the inflammatory mediator IL-6. Later, the anti-inflammatory cytokine IL-10 is produced as the body attempts to control the systemic inflammatory response. The systemic increase in IL-10 following a cytokine storm is a marker of a counter-anti-inflammatory response called “immunoparalysis”, associated with downregulation of neutrophil and monocyte function. Patients who do not die as a result of the initial cytokine storm but subsequently die may be those who don’t recover from immunoparalysis (Tisoncik et al. 2012).
Some people seem particularly susceptible to the cytokine storm, while others seem relatively resistant. This could be caused by underlying genetic differences, including differences in the toll-like receptor (TLR) structure and function. Variants of TLR4, for example, can predispose people to sepsis (Tisoncik et al. 2012). Studies have also revealed risk factors for sepsis including age (under 1 year or over 75 years), immunosuppression (for example people with diabetes, or people receiving chemotherapy or immunosuppressive drugs), and recent surgery or invasive procedure (NICE guideline NG51). Identifying risk factors for the cytokine storm within COVID-19 infection might help healthcare professionals to manage patients and find the best outcomes.
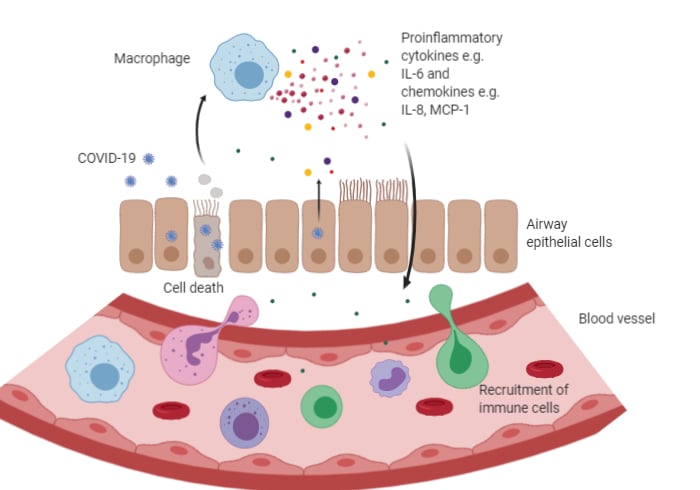
Fig.1. Cytokine storm overview Infection by a virus like COVID-19 leads to cell death and subsequent macrophage activation. Activated macrophages release pro-inflammatory cytokines, leading to the destruction of epithelial cell contacts. This is accompanied by the release of chemoattractant cytokines to recruit more immune cells. These immune cells also release more cytokines. More cytokines are released by infected cells through activation of NFκB pathway. Activation of an increasing number of immune cells and further uncontrolled cytokine release leads to hyperinflammation and cellular damage.
COVID-19 and Cytokine Storms
ARDS is the leading cause of death in patients with SARS-CoV or MERS-CoV, so it’s unsurprising that it is also an important factor in deaths resulting from SARS-CoV-2. Many of the patients who have become critically ill or died as a result of COVID-19 have experienced rapid deterioration during the later stages of their disease or during recovery, while many have experienced rapid ARDS and multiple organ failure and died quickly (Ye et al. 2020). These observations are consistent with a cytokine storm being an integral factor in their deterioration and death.
Recent studies have analyzed the cytokine profiles in patients with COVID-19, to shed some light on the specifics of an overactive response. High levels of inflammatory cytokines have been identified in patients with COVID-19, including IL-1B, IFN-γ, IP-10, and MCP-1. One study compared the cytokine profiles of ICU patients against non-ICU patients and found that ICU patients had higher levels of various cytokines (Ye et al. 2020). Research into the exact cytokine profiles of patients hospitalized with COVID-19 is still in its early days but offers hope that we may be able to reduce the number of deaths.
Can We Prevent or Treat COVID-19 Cytokine Storms?
Several ideas have been proposed to try and treat/prevent cytokine storms, and scientists are rapidly working to collect data and publish findings so that cures may be verified as quickly as possible. A major therapeutic goal for COVID-19 treatment is to repurpose existing drugs as they have the potential to get to patients much faster (Wu and Yang 2020). The speed of the pandemic creates urgency: patients, governments and healthcare authorities need solutions now, and developing new treatments will take years.
Blocking IL-6 has been suggested as a method for treating the cytokine storm in COVID-19 patients. IL-6 is rapidly synthesized as part of the cytokine storm, and levels of IL-6 are a predictor of mortality in COVID-19 patients (Rizzo et al. 2020). Two monoclonal antibodies that inhibit the IL-6 receptor, therefore blocking IL-6 function, are already licensed for treating autoimmune disorders, including tocilizumab. Multiple clinical trials aim to assess the effectiveness of IL-6 receptor inhibitors for patients with severe SARS-CoV-2 pneumonia (Rizzo et al. 2020).
Melatonin is an anti-inflammatory, anti-oxidative molecule which is protective against ALI/ARDS caused by other viruses and pathogens, and has a high safety profile. The use of melatonin as an adjuvant for treating COVID-19 patients has been suggested (Zhang R et al. 2020). In addition, the MeCOVID trial will assess the efficacy of melatonin for prevention of COVID 19 infection among healthcare workers (ClinicalTrials.gov NCT04353128).
Corticosteroids are used to suppress inflammation and have been suggested as treatments for the COVID-19 cytokine storm. Some evidence from a previous outbreak is encouraging – when used properly, corticosteroids significantly reduced mortality and shortened the hospital stay during the 2003 SARS epidemic. However, other studies during the 2003 SARS outbreak suggested that adverse events or delayed viral clearance as a result of glucocorticoid use led to deterioration (Zhang W et al. 2020). It is unknown whether corticosteroids should be routinely used for some patients with COVID-19 (Zhang W et al. 2020).
It is important to note that attempts to dampen the immune response might backfire (Tisoncik et al. 2012). Immune responses can change quickly during an infection and the interventions needed earlier might be completely different from interventions needed only a few hours later. Treating patients with an immunosuppressant when their immune system is still battling to fight the virus could have disastrous effects.
Scientists are accelerating their efforts to understand cytokine storms in relation to COVID-19 and moving forward with impressive speed. Hopefully, by pulling together and working hard, the best treatments will be found for hospitalized patients with COVID-19 as quickly as possible.
References
ClinicalTrials.gov NCT04353128, Efficacy of melatonin in the prophylaxis of coronavirus infectious disease 2019 (COVID-19) among healthcare workers (The MeCOVID Study). (MeCOVID).
Estes C (2020). What is the cytokine storm and why is it so deadly for coronavirus patients? Forbes. Accessed on 04/28/2020
Goodman B (2020). Cytokine storms may be fueling some COVID deaths. WebMD Health News 17 April 2020. Accessed on 04/28/2020
Guo XJ and Thomas PG (2018). New fronts emerge in the influenza cytokine storm, Semin Immunopathol 39, 541–550.
NICE guideline NG51 (2017). Sepsis: recognition, diagnosis and early management. Available at: www.nice.org.uk/guidance/ng51/chapter/recommendations#risk-factors-for-sepsis. Accessed 04/28/2020
Rizzo P et al. (2020). COVID-19 in the heart and the lungs: could we “Notch” the inflammatory storm? Basic Res Cardiol 115, 31.
Tisoncik JR et al. (2012). Into the eye of the cytokine storm. Microbiol Mol Biol Rev 76, 16–32.
Wu D and Yang XO (2020). TH17 responses in cytokine storm of COVID-19: An emerging target of JAK2 inhibitor Fedratinib. J Microbiol Immunol Infect Epub ahead of print.Accessed 04/28/2020
Ye Q et al. (2020). The pathogenesis and treatment of the `cytokine storm' in COVID-19. J Infect Epub ahead of print. Accessed 04/28/2020
Zhang R et al. (2020). COVID-19: Melatonin as a potential adjuvant treatment, Life Sci 250: 117583.
Zhang W et al. (2020). The use of anti-inflammatory drugs in the treatment of people with severe coronavirus disease 2019 (COVID-19): The experience of clinical immunologists from China. Clin Immunol Epub ahead of print. Accessed 04/28/2020
You may also be interested in...

View more Immunology or Article blogs















