
Popular topics

-
References
Abramyan S and Hanlon M. (2023). Kidney transplantation. Available from: StatPearls [Internet].
Anand RP et al. (2023). Design and testing of a humanized porcine donor for xenotransplantation. Nature 622, 393-401.
Chen TK et al. (2019). Chronic kidney disease diagnosis and management. JAMA 322, 1,294-1,304.
Groth CG. (2007). The potential advantages of transplanting organs from pig to man: A transplant surgeon's view. Indian J Urol 23, 305-309.
Hashmi MF et al. (2023). End-stage renal disease. Available from: StatPearls [Internet].
Justiz Vaillant AA and Mohseni M. (2023). Chronic transplantation rejection. Available from: StatPearls [Internet].
Kozlov M. (2023). Monkey survives for two years after gene-edited pig-kidney transplant. Nature 622, 437-438.
Wang R et al. (2019). Antigenicity of tissues and organs from GGTA1/CMAH/β4GalNT2 triple gene knockout pigs. J Biomed Res 33, 235-243.
Xi J et al. (2022). Genetically engineered pigs for xenotransplantation: hopes and challenges. Front Cell Dev Biol 10, 1093534.
Zhou Q et al. (2022). Current status of xenotransplantation research and the strategies for preventing xenograft rejection. Front Immunol 13, 928173.
Can Designer Pigs Improve Xenotransplantation?
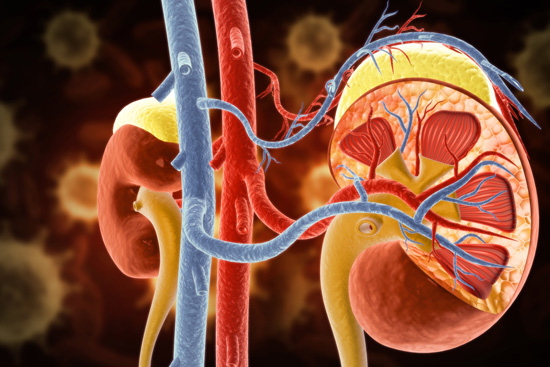
Chronic kidney disease (CKD) is an umbrella term describing the progressive loss of kidney function over time. This can be attributed to a range of conditions, such as hypertension or diabetes, which significantly impair the ability of the kidneys to filter waste products from the blood (Chen et al. 2019). The terminal stage of CKD is known as end-stage renal disease (ESRD), and over 500,000 people live with this deadly and debilitating condition in the US alone (Hashmi et al. 2023).
While dialysis can treat the symptoms and extend the life expectancy of a patient with CKD, it is a less-than-ideal treatment option due in large part to the time constraints it places on the individual, often carried out three days a week for around four hours per session. Kidney transplantation is considered the gold standard treatment for many patients, significantly ameliorating the quality of life and improving survival, with a projected ten year increase in life span compared to dialysis (Abramyan and Hanlon, 2023). Unfortunately, a shortage of viable organs considerably limits the lifesaving impact of transplantation. According to the National Kidney Foundation, the average wait time for a kidney transplant is between 3-5 years. Regrettably, many patients die or deteriorate in health to the point where they are no longer eligible for the surgery during this time.
One potential solution to the scarcity of suitable human organs is using pig kidneys, a process known as xenotransplantation. In this blog, we will discuss recent advances in the development of transplant-ready pig kidneys as a source of lifesaving organs for ESRD patients.
Pig Problems
You may be wondering: why pigs? Well, it turns out that the physiological metabolism and immune system of pigs are strikingly similar to that of humans (Xi et al. 2022). Not only that, but millions of pigs are slaughtered each year for meat consumption, and their organs largely go unused, meaning there are potentially millions of unused kidneys going to waste (Groth 2007). So, if we just use these tissues for transplantation that would solve the organ shortage problem, right? Unfortunately, it’s not that simple.
One of the main problems associated with xenotransplantation is the risk of rejection. This can be further subclassified as hyperacute, acute, and chronic rejection. Hyperacute rejection occurs within 24 hours of grafting and is caused by preexisting antibodies in the recipient that target antigens of the donor, subsequently activating the complement cascade and attacking the graft via the innate immune system.
In contrast, acute rejection involves the adaptive immune system, when specific lymphocytes are produced that target the antigen-presenting molecules, known as the major histocompatibility complex (MHC) (or human leukocyte antigen (HLA) in humans), on the cell surface of the graft. Due to the involvement of the adaptive response, this typically takes longer, occurring days to weeks after grafting.
Finally, chronic rejection can occur months to years after the transplantation. Currently, the mechanisms behind chronic rejection are poorly understood. However, research suggests that it involves both immune factors, such as targeting of MHC as with acute rejections, and non-immune factors, for example, incompatibilities in coagulation factors of the two species (Justiz Vaillant and Mohseni 2023, Zhou et al. 2022).
An additional issue accompanying xenotransplantation is the threat of infection, particularly, by porcine endogenous retrovirus (PERV). Using pigs from strictly controlled herds can minimize the risk of infection from most pathogens. PERV, however, poses a specific danger as it is a permanent part of the porcine genome. In the pig, this endogenous virus is typically harmless and fails to replicate under physiological conditions. However, whether or not infection would reignite after using the graft organ to piggyback into the human remains unknown (Groth 2007).
But rather than give up on this untapped supply of lifesaving organs, scientists have come up with a potential solution: genetic engineering of donor pigs to circumvent these issues. In a recent study by Anand et al. (2023), researchers made a grand total of 69 genomic edits in pigs before assessing the success of kidney transplantation into monkeys.
Better by Design
The most prominent hurdles to overcome in xenotransplantation are the risk of rejection and infection. The three major glycan antigens expressed on the cell surface of porcine cells are galactose-α1,3-galactose (αGal), N-glycolylneuramine acid (Neu5Gc), and Sia-α2.3-[GalNAc-β1.4]Gal-β1.4-GlcNAc (Sd(a)), which provoke hyperacute rejection of the graft by preformed antibodies in the recipient (Wang et al. 2019). Therefore, it will come as no surprise that enzymes associated with the synthesis of these three molecules were amongst the genes targeted in the editing masterplan of the scientists. Additionally, a substantial 59 edits were performed to inactivate the PERV elements present in the genomes of the donor pigs.
The remaining seven edits were the addition of human transgenes to the pig to aid in the maintenance of the organ once in the recipient monkey. Specifically, the genes included were CD46 and CD55 to diminish the activation of the complement cascade; THBD and PROCR to prevent unwanted blood coagulation; CD47, which works as a “don’t eat me” signal to macrophages; and TNFAIP3 and HMOX1 to reduce any potential ischemia-reperfusion injury, apoptosis, and inflammation.
Monkey Business
Pigs with all the rejection-related, PERV-inactivating, and human transgene edits were bred alongside control pigs with different combinations of these edits. Kidneys from the animals were then transplanted into cynomolgus macaques to evaluate the efficacy of the altered organs as grafts.
Interestingly, the monkeys that received kidneys with rejection-related and PERV-inactivating edits but no human transgenes did not survive longer than 50 days posttransplant. Conversely, those that received kidneys with both rejection-related and human transgene edits achieved significantly longer survival, with 9 of the 15 monkeys surviving longer than 50 days, five of which survived for over a year, and one monkey who survived over two years for a whopping 758 days. Notably, whether or not the graft included PERV-inactivating gene edits didn’t appear to make a difference to the overall survival of the animal.
Some scientists believe the number of gene modifications performed in this study was excessive, stating that each edit will render the technique more difficult to reproduce and scale up (Kozlov 2023). Interestingly, the longest case of a genetically modified pig kidney functioning in a human has recently been documented. In this instance, just one single edit was made to the genome of the donor, to inhibit the production of αGal, and the pig’s thymus was transplanted alongside the kidney to help reduce the risk of rejection. The family of a man who had been declared brain-dead donated his body for the experiment after learning that his organs were not eligible for donation due to the aggressive form of brain cancer that he suffered from. Upon transplantation, the kidney remained functional for the entire 61 day experiment, with only a subtle sign of rejection onset after one month, which was quickly remedied with an alteration in the immunosuppressants administered.
So, while scientists will still need to figure out how much or how little genetic engineering of pigs is necessary to achieve the optimal result in humans, the results of the research by Anand et al. give hope that science is getting closer and closer to bringing home the bacon when it comes to xenotransplantation.
Do You Work in Pig Research?
Bio-Rad offers a range of porcine antibodies that target CD markers, cytokines, and immunoglobulins, as well as recombinant porcine cytokines to help you study immune responses in pigs.
References
Abramyan S and Hanlon M. (2023). Kidney transplantation. Available from: StatPearls [Internet].
Anand RP et al. (2023). Design and testing of a humanized porcine donor for xenotransplantation. Nature 622, 393-401.
Chen TK et al. (2019). Chronic kidney disease diagnosis and management. JAMA 322, 1,294-1,304.
Groth CG. (2007). The potential advantages of transplanting organs from pig to man: A transplant surgeon's view. Indian J Urol 23, 305-309.
Hashmi MF et al. (2023). End-stage renal disease. Available from: StatPearls [Internet].
Justiz Vaillant AA and Mohseni M. (2023). Chronic transplantation rejection. Available from: StatPearls [Internet].
Kozlov M. (2023). Monkey survives for two years after gene-edited pig-kidney transplant. Nature 622, 437-438.
Wang R et al. (2019). Antigenicity of tissues and organs from GGTA1/CMAH/β4GalNT2 triple gene knockout pigs. J Biomed Res 33, 235-243.
Xi J et al. (2022). Genetically engineered pigs for xenotransplantation: hopes and challenges. Front Cell Dev Biol 10, 1093534.
Zhou Q et al. (2022). Current status of xenotransplantation research and the strategies for preventing xenograft rejection. Front Immunol 13, 928173.
You may also be interested in...

View more Veterinary or Article blogs















