
Popular topics

-
References
Baruch E at al. (2021). Fecal microbiota transplant promotes response in immunotherapy-refractory melanoma patients. Science 371, 602-609.
Choi Y et al. (2023). Immune checkpoint blockade induces gut microbiota translocation that augments extraintestinal antitumor immunity. Sci Immunol 8, eabo2003.
Derosa L et al. (2018). Negative association of antibiotics on clinical activity of immune checkpoint inhibitors in patients with advanced renal cell and non-small-cell lung cancer. Ann Oncol 29, 1,437-1,444.
Larkin J et al. (2019). Five-year survival with combined nivolumab and ipilimumab in advanced melanoma. N Engl J Med 381, 1,535-1,546.
Tiny Gut Microbes Boost the Immune System to Fight against Cancer
Immune checkpoints are essential regulatory mechanisms present in specific immune cells, particularly in T cells. These checkpoints involve the recognition of proteins, such as PD-1 or B7-1/B7-2 (also known as CD80/CD86), on the surface of other cells, acting as negative regulators of immune responses to prevent prolonged inflammation and maintain self-tolerance.
Strikingly, cancer cells can exploit these checkpoints to evade immune surveillance. By overexpressing checkpoint proteins such as PD-1, cancer cells can not only put the brakes on the immune response, but effectively evade detection and destruction by T cells.
Fortunately, scientists have developed a treatment known as immune checkpoint blockade therapy (ICT). This therapy utilizes drugs capable of inhibiting checkpoint proteins such as PD-1 and CTLA-4 (the B7-1/B7-2 receptor). By employing ICT, T cells can release their brake, enabling them to detect and eradicate tumor cells. Essentially, this treatment, also known as immunotherapy, leverages a patient’s own immune cells to combat cancer.
While ICT has revolutionized cancer treatment, over 50 percent of patients fail to respond to immunotherapy, indicating the efficacy of ICT varies across individuals (Larkin et al. 2019). A recent study published by Choi et al. (2023) points to a potential influence on immunotherapy outcomes: the gut bacteria. This study underscores a connection between gut microbes and ICT effectiveness. In this blog, we will delve into how these microorganisms residing in our intestines can impact the anti-tumor response triggered by ICT.
Gut Microbiota: Friends or Foes?
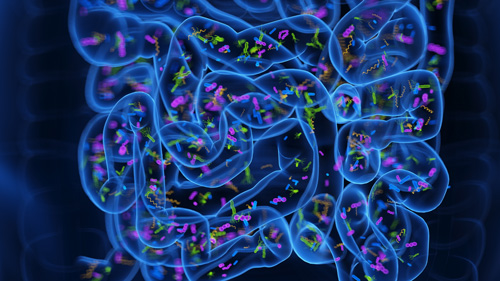
Our human body serves as a host for trillions of microorganisms, referred to as microbiota. These microbes have a profound impact on human health and disease. For instance, microbes residing in our gut play crucial roles in various physiological functions, including digestion, metabolism, and immune system development. While many strains are beneficial, aiding in nutrient absorption and pathogen resistance, others can become opportunistic pathogens under certain conditions, leading to infections or dysbiosis.
So, the question is, can gut microbes change therapeutic response to treatment for diseases like cancer?
ICT Can Promote the Migration of Gut Microbes
Previous studies have reported gut microbiota can impact the effect of cancer immunotherapy. For instance, fecal microbiota transplant has been shown to improve the efficacy of anti–PD-1 immunotherapy in melanoma patients (Baruch et al., 2021). Nevertheless, how gut microbiota can enhance the anti-cancer response in tumors from a distant site in the body remains unclear. To address this question, the researchers from The University of Texas Southwestern Medical Center utilized a preclinical melanoma mouse model to study how gut microbes can increase the efficiency of anti-PD-1/CTLA-4 therapy.
When mice implanted with melanoma cells underwent ICT treatment, the study group observed an increased number of gut bacteria traveling to both tumors and secondary lymphoid organs (e.g., lymph nodes, spleen). The researchers further examined the composition of gut microbiota translocated to secondary lymphoid organs and noted that Enterococcus faecalis and Lactobacillus johnsonii were the two most abundant gut bacteria to migrate to the secondary lymphoid organs after two doses of ICT.
So how do these translocated bacteria from the gut activate anti-cancer immunity upon administration of ICT?
The group hypothesized that gut bacteria translocated to secondary lymphoid organs can lead to the activation of dendritic cells (DC) and subsequently promote effector T cell responses against tumor cells. Consistent with this, when DCs were stimulated ex vivo with the previously identified strains of gut bacteria, a higher abundance of activated DCs, marked by high expression of MHCII/CD40/CD80, was observed. Moreover, CD8+ T cells primed with those activated DCs also had higher interferon-γ (IFN-γ) production.
Next, the scientists tested which of the secondary lymphoid organs accounted for the enhanced anti-cancer immunity induced by ICT. Notably, upon surgical resection of mesenteric lymph nodes (MLN), a secondary lymphoid organ in the intestine, the researchers observed increased tumor growth and reduced survival rate in melanoma-implanted mice receiving ICT.
To further gain insight into how gut microbes migrate to secondary lymphoid organs, the researchers tested if DCs are required for this translocation. They utilized a transgenic mouse that expresses the diphtheria toxin receptor only in cells which express CD11c, a common dendritic cell marker. Hence, upon administration of diphtheria toxin, only CD11c-expressing cells are vulnerable and will be depleted.
Indeed, depletion of DCs in melanoma-implanted mice led to a reduction in the amount of gut microbes translocated to secondary lymphoid organs upon ICT treatment. Furthermore, the study group also found ICT treatment in melanoma-implanted mice can induce MLN remodeling, anatomical changes within lymph nodes to allow immune cell infiltration. Collectively, these data suggest gut bacteria translocation to the distal locations near the tumor is mediated by both DCs and MLN remodeling.
Manipulation of Gut Microbiota Can Affect Anti-Cancer Response
Antibiotic treatment has been linked to poor clinical outcomes for cancer patients undergoing ICT therapy (Derosa et al. 2018). To further investigate the underlying mechanisms for this observation, the researchers administered ICT-treated melanoma-implanted mice with antibiotics. Notably, both the abundance of gut microflora translocated to secondary lymphoid organs and effector CD8+ T cell responses were reduced in the antibiotics-treated groups. The overall efficacy of ICT is also decreased in melanoma-implanted mice treated with antibiotics. These data further demonstrated that the alteration of gut microbiota composition can reduce the anti-cancer immune response induced by ICT.
Together, this study provides novel insights into advancing cancer treatment. By elucidating the impact of gut bacteria on immune responses triggered by ICT, it not only aims to improve ICT efficacy for patients, but might shed light on the development of personalized medicine for cancer patients.
Are You Interested in Studying Cancer?
Check out Bio-Rad’s range of antibodies, proteins, and reagents for cancer research.
References
Baruch E at al. (2021). Fecal microbiota transplant promotes response in immunotherapy-refractory melanoma patients. Science 371, 602-609.
Choi Y et al. (2023). Immune checkpoint blockade induces gut microbiota translocation that augments extraintestinal antitumor immunity. Sci Immunol 8, eabo2003.
Derosa L et al. (2018). Negative association of antibiotics on clinical activity of immune checkpoint inhibitors in patients with advanced renal cell and non-small-cell lung cancer. Ann Oncol 29, 1,437-1,444.
Larkin J et al. (2019). Five-year survival with combined nivolumab and ipilimumab in advanced melanoma. N Engl J Med 381, 1,535-1,546.
You may also be interested in...

View more Immunology or Cancer blogs















