
Popular topics
-
References
Wattananit S et al. (2016). Monocyte-derived macrophages contribute to spontaneous long-term functional recovery after stroke in mice. J Neuroci 36, 4182-4195.
van de Laar L et al. (2016). Yolk sac macrophages, fetal liver, and adult monocytes can colonize an empty niche and develop into functional tissue resident macrophages. Immunity 44, 755-768.
Thèriault P et al. (2015). The dynamics of monocytes and microglia in Alzheimer’s disease. Alzheimer’s Res Ther 7, 41.
Shechter R et al. (2013). Recruitment of beneficial M2 macrophages to injured spinal cord is orchestrated by remote brain choroid plexus. Immunity 38, 555-569.
Monocyte-based cell therapy for treating diseases
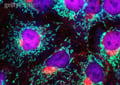
The transplantation of blood stem cells to treat blood and immunological diseases is the most well-established and widely used form of stem cell therapy. This treatment strategy relies on the ability of stem cells to differentiate into specific cell types that perform specialized functions to ultimately treat or prevent disease. Similar to stem cell therapy, the results of recent pre-clinical studies suggest that monocytes could be applied in a related manner to the treatment of stroke (Wattananit et al. 2016) or rare diseases such as pulmonary alveolar proteinosis (PAP, van de Laar et al. 2016).
Monocytes and stroke
Up until recently, scientists believed that inflammation in the damaged part of the brain after a stroke was a negative consequence to be resolved as soon as possible. However, researchers at the Lund Stem Cell Center, demonstrated that inflammatory cells, particularly monocytes, that infiltrate the brain after a stroke are in fact necessary for initiating long-term spontaneous recovery (Wattananit et al. 2016). Using a mouse model of stroke, they demonstrate that once in the brain, monocytes differentiate into anti-inflammatory macrophages that clear the dead nerve cell tissue and secrete anti-inflammatory molecules that help the brain to repair the damage.
Current treatment strategies for stroke involve dissolving or removing the blood clot that caused the stroke. However, such strategies are only effective if applied in the very early stages after an insult. The recent findings showing the reparative function of monocyte derived macrophages suggests that a new treatment strategy for stroke patients could involve increasing the number of monocytes in the injured brain through monocyte engraftment. The researchers show that monocyte infiltration to the brain peaks 3 days after a stroke, indicating that the proposed monocyte-based cell therapy could likely be administered within a few days of an insult to assist in the repair of damaged brain tissue (Wattananit et al. 2016).
Monocytes and PAP
Other scientists at the Flanders Institute for Biotechnology-Ghent University (VIB-UGent) have tested the feasibility of monocyte-based cell therapy for the treatment of PAP (van de Laar et al. 2016). PAP is a rare blood disease characterized by a lack of alveolar macrophages in the lungs. Alveolar macrophages maintain lung homeostasis by clearing pulmonary surfactant, and defective clearance of surfactant in the lungs leads to PAP. In a mouse model of PAP, these researchers demonstrated that a single transfer of fetal-liver monocytes (FL-MO), bone-marrow derived monocytes (BM-MO) or yolk sac macrophages (YS-Mac) led to complete replenishment of alveolar macrophages in the lungs (van de Laar et al. 2016). These adult circulating monocytes (FL-MO and BM-MO) and embryonic precursors (YS-Mac) independently differentiated into fully functional and self maintained alveolar macrophages that prevented PAP in mice for up to one year (van de Laar et al. 2016).
Monocyte-based cell therapy
These pre-clinical studies pave the way for monocyte-based cell therapy as a means of treating diseases in which monocytes and macrophages play key roles, such as spinal cord injury (Shechter et al. 2013) and Alzheimer’s disease (Thèriault et al. 2015) . Since circulating monocytes (FL-MO and BM-MO) are accessible from the blood, this strategy could easily be administered in a clinical setting, and is therefore extremely promising. However, future studies investigating the clinical application of monocyte-based cell therapy should explore appropriate timing of monocyte administration in particular disease contexts as well as how to manage possible negative outcomes such as chronic inflammation.
Interested in monocytes?
To learn more about monocyte development and their role in disease, check out our latest monocyte mini-review.
References
Wattananit S et al. (2016). Monocyte-derived macrophages contribute to spontaneous long-term functional recovery after stroke in mice. J Neuroci 36, 4182-4195.
van de Laar L et al. (2016). Yolk sac macrophages, fetal liver, and adult monocytes can colonize an empty niche and develop into functional tissue resident macrophages. Immunity 44, 755-768.
Thèriault P et al. (2015). The dynamics of monocytes and microglia in Alzheimer’s disease. Alzheimer’s Res Ther 7, 41.
Shechter R et al. (2013). Recruitment of beneficial M2 macrophages to injured spinal cord is orchestrated by remote brain choroid plexus. Immunity 38, 555-569.
You may also be interested in...
View more Immunology or Science News blogs















