
Popular topics

-
References
Asano K et al. (2011). CD169- Positive macrophages dominate antitumor immunity by crosspresenting dead cell-associated antigens. Immunity 34, 85-95.
Beatty GL et al. (2011). CD40 agonists alter tumor stroma and show efficacy against pancreatic carcinoma in mice and humans. Science 331, 1612-1616.
Long KB et al. (2016). IFN-gamma and CCL2 cooperate to redirect tumor-infiltrating monocytes to degrade fibrosis and enhance chemotherapy efficacy in pancreatic carcinoma. Cancer Discov pii: CD-15-1032 [Epub ahead of print].
Mills CD et al. (2016). A breakthrough: Macrophage-directed cancer immunotherapy. Cancer Res 76, 513-516.
O’Sullivan T et al. (2012). Cancer immunoediting by the innate immune system in the absence of adaptive immunity. J Exp Med 209, 1869-1882.
Inducing macrophages that work against rather than for cancer
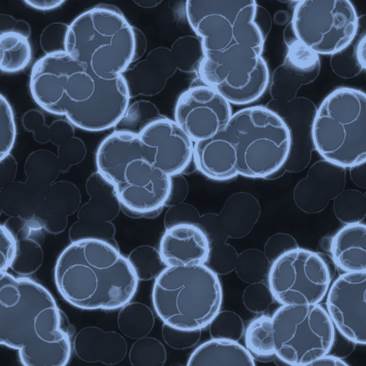
Within the immune response to cancer, macrophages present both a potential problem, and a potential solution. This is primarily because within the tumor microenvironment (TME), macrophages come in many flavors. There are M1/kill-type macrophages that can slow or stop tumor growth, M2/repair-type macrophages that produce growth stimulating molecules that promote tumor progression (Mills CD et al. 2016) as well as CD169+ macrophages that can activate adaptive anti-tumor immune responses (Asano K et al. 2011). Upon recruitment by a growing tumor, monocytes (macrophage precursors) are primarily driven towards differentiation into M2/repair-type macrophages by cytokines within the TME. Consequently, M2/repair-type macrophages predominate in the TME and promote tumor growth and metastasis. Scientists are however devising strategies to drive monocytes to differentiate into M1/kill-type macrophages that can assist in tumor clearance. Studies have shown that increasing the presence of these killer macrophages in the TME is sufficient to cause tumor rejection in vivo (O’Sullivan T et al. 2012, Mills CD et al. 2016).
Switching macrophage differentiation
One way of achieving this switch in differentiation to the M1/killer phenotype is through the use of immunotherapeutic drug molecules. Immunotherapeutic approaches to cancer therapy such as the immune checkpoint antibody drugs anti-cytotoxic T lymphocyte antigen 4 (CTLA-4) and anti-programmed death 1 (PD1) have demonstrated significant success in treating cancers, particularly melanoma. However, they have primarily been reported to mediate their effects through T cell activation. In contrast, a study by Beatty GL et al. (2011) demonstrated that administration of an agonist CD40 antibody induced tumor regression in a pancreatic ductal adenocarcinoma (PDA) mouse model, and the effect was independent of T cells but was contingent on the activity of macrophages.
The mechanism responsible for this effect was reported in a recent study by the same research group, and it turns out that it requires increasing the number of M1/killer type macrophages in the TME (Long KB et al. 2016). The authors showed that M1 promoting molecules IFN-gamma and CCL2, released systematically in response to the CD40 agonist antibody, cooperated to induce this effect. CCL2 mediated the infiltration of monocytes into the TME and IFN-gamma was responsible for promoting M1/killer type macrophage differentiation within the tumor. Consequently, these M1 killer macrophages attacked the cancer by releasing key metalloproteinases, which are enzymes that degrade the fibrotic scaffold surrounding tumors. This scaffold protects tumors from chemotherapy, therefore the effect of CD40 activation on directing macrophages to the M1 killer phenotype led to enhanced chemotherapy efficacy.
A new way for cancer therapy?
This study provides further experimental evidence supporting a new way forward in cancer therapy. Prior research efforts focused on eliminating cancer promoting M2/repair-type macrophages, but the proposed new strategy of forcing monocytes to differentiate to the M1/killer phenotype is considered a “breakthrough” in cancer immunotherapy (Mills CD et al. 2016). However, there are significant drawbacks to this approach that need to be addressed. It has been reported that overzealous M1/killer-type responses can lead to atherosclerosis and other chronic inflammatory conditions. Therefore, future efforts to manage or prevent these side effects are an important next step in moving this pre-clinical observation into the clinic.
Studying macrophage subsets?
For more details on the various macrophage subsets, and the mechanisms that drive their differentiation to certain phenotypes, check out our new macrophage polarization mini-review.
References
Asano K et al. (2011). CD169- Positive macrophages dominate antitumor immunity by crosspresenting dead cell-associated antigens. Immunity 34, 85-95.
Beatty GL et al. (2011). CD40 agonists alter tumor stroma and show efficacy against pancreatic carcinoma in mice and humans. Science 331, 1612-1616.
Long KB et al. (2016). IFN-gamma and CCL2 cooperate to redirect tumor-infiltrating monocytes to degrade fibrosis and enhance chemotherapy efficacy in pancreatic carcinoma. Cancer Discov pii: CD-15-1032 [Epub ahead of print].
Mills CD et al. (2016). A breakthrough: Macrophage-directed cancer immunotherapy. Cancer Res 76, 513-516.
O’Sullivan T et al. (2012). Cancer immunoediting by the innate immune system in the absence of adaptive immunity. J Exp Med 209, 1869-1882.
You may also be interested in...
















