
Popular topics

-
References
Allen G et al. (2022). Synthetic cytokine circuits that drive T cells into immune-excluded tumors. Science 378, eaba1624.
June C et al. (2018). CAR T cell immunotherapy for human cancer. Science 359, 1361-1365.
Larson R and Maus M. (2021). Recent advances and discoveries in the mechanisms and functions of CAR T cells. Nat Rev Cancer 21, 145-161.
Li H et al. (2022). Multidimensional control of therapeutic human cell function with synthetic gene circuits. Science 378, 1227-1234.
Sterner R and Sterner R. (2021). CAR-T cell therapy: current limitations and potential strategies. Blood Cancer J 11, 69.
Immune Cells Get an Upgrade: A Stronger Defense against Cancer
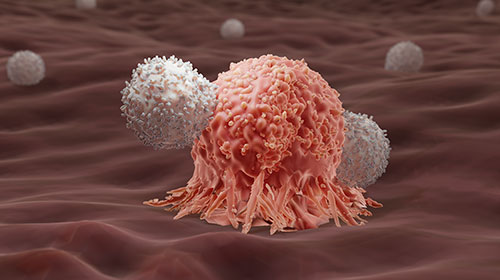
To protect the body from intruders, our immune system has the ability to distinguish self from non-self. Detection of non-self antigens, molecules, or foreign substances that trigger an immune response is a key step for the clearance of invading pathogens by immune cells. Remarkably, our immune cells can also differentiate tumor cells from normal cells by recognizing distinct antigens on cancer cells.
By leveraging the concepts of synthetic biology, scientists have engineered T cells to fight against cancer via the recognition of these tumor antigens. These engineered immune cells led to the development of an innovative cancer therapy termed chimeric antigen receptor (CAR) T-cell therapy.
However, despite the breakthrough of CAR T-cell therapy, several challenges have emerged, prompting the need to seek additional strategies to improve this treatment. For instance, CAR T-cell therapy can lead to a systemic inflammatory response, due to the release of excessive signaling molecules, called cytokines, from these engineered immune cells (Larson and Maus 2021).
A new study published by Li et al. (2022) in Science reports that researchers designed CAR T cells in a way that allows both the release of cytokines and expression of CARs to be controlled by different clinically approved drugs.
What are CAR T cells?
CAR T cells are patient-derived T cells manipulated to express synthetic receptors (CARs) that target specific antigens on cancer cells.
CARs span the membrane of these genetically modified T cells and consist of two components. The extracellular part of the CAR contains the variable regions of the antibody that can recognize antigens on tumor cells. The intracellular portion is composed of co-stimulatory signaling and activation domains required to activate T cells (June et al. 2018).
Currently, CAR T-cell therapy has been primarily used to treat leukemia. In fact, the US Food and Drug Administration (FDA) approved the first series of commercial CAR T-cell therapies for multiple types of leukemia in 2017 (Sterner and Sterner 2021).
Researchers Upgrade the Functionality of CAR T-cells
Despite the convenience of electronic devices, such as iPhones, they can still experience bugs and glitches that can cause problems for users. To overcome those issues, software updates are often required to improve the functionality and performance of the system. Similarly, while CAR T-cell therapy is a transformative treatment for cancer patients, continued advancement is necessary to increase its therapeutic effectiveness and minimize associated risks.
To increase the efficacy of CAR T-cell therapy, a research group from Boston University generated an updated version of CAR T cells to enhance their antitumor activity with limited toxicity to the recipients.
So how can scientists upgrade CAR T cells to safely and effectively target cancer cells?
In order to improve the performance of CAR T cells, the researchers developed an artificial gene regulator, which they called a synthetic zinc finger transcription regulator (synZiFTR), to control the function of these engineered T cells via transcriptional regulation.
The synZiFTR consists of two different human-derived protein domains. One part of the regulator contains a small zinc finger portion- a DNA-binding domain commonly found in transcription factors. The other region is composed of a p65 protein domain to allow activation of gene transcription.
The researchers built a series of synZiFTRs, which could each bind unique genetic sequences called DNA binding motifs (DBM) to induce the expression of a specific downstream gene. The scientists then constructed synthetic gene circuits by introducing synZiFTRs into cells via lentiviral transduction. Analysis of the artificial gene circuits showed a high specificity of each synZiFTR to its associated DBM and targeted gene without nonspecific interference with the regulation of other native gene expression.
Next, the team built a gene switch in the artificial gene circuit to further regulate gene expression. Each selected synZiFTR was fused with an additional protein domain that can be bound by a specific FDA-approved compound such as grazoprevir (an antiviral drug) or tamoxifen (a breast cancer drug). Therefore, due to the new design of the genetic regulator, activation of synZiFTR can only occur in the presence of these small molecules. In other words, the expression of a particular gene can only be switched to the “on” state after treatment with drugs.
Lastly, the research group implemented this synthetic gene circuit in CAR T-cell therapy. They developed a dual-switch gene circuit by building two different genetic regulators in CAR T cells specific for Her2, a protein that is overexpressed in cancers such as leukemia. This dual-switch gene circuit enables the induction of the CAR and interleukin-2 (IL-2), a cytokine that stimulates T cells but can cause serious adverse effects in high doses, by two separate compounds (grazoprevir and tamoxifen), respectively (Figure 1). Strikingly, when these genetically engineered CAR T cells were transferred into a mouse model of leukemia, sequential administration of tamoxifen and grazoprevir enhanced the ability of these programmable T cells to reduce tumor burden and ultimately prolong survival. The data further demonstrated that expression of CAR or IL-2 alone has limited efficacy for the eradication of cancer cells, whereas synergistic activation of both genes in CAR T cells can improve the antitumor response of these immune cells.
Upgraded CAR T Cells Effectively Attack Cancer Cells with High Precision
While CAR T-cell therapy has revolutionized cancer treatment for patients, the precise delivery of antitumor cytokines, such as IL-2, from these cells remains a limitation. This study addresses this issue by building gene switches that precisely control the activities of CAR T cells in a timely and safe manner. Likewise, another independent study by Allen et al. (2022) in Science also showed CAR T cells can effectively eliminate pancreatic cancer cells by inducing IL-2 expression with a different gene circuit called synNotch. Taken together, both studies developed new therapeutic approaches to combat cancer and advance CAR T-cell therapy by equipping these programmable T-cells with multiple tools.

Fig. 1. The upgraded CAR T cell with a dual-switch genetic circuit can effectively kill cancer cells. Treatment with two separate small molecules can control the expression of CAR and IL-2 through two distinct gene circuits. Grazoprevir: GZV. Tamoxifen:4OHT/TMX.
Working with CAR T Cells?
Take a look at our resource to find out how to optimize your CAR T cell workflow using flow cytometry.
References
Allen G et al. (2022). Synthetic cytokine circuits that drive T cells into immune-excluded tumors. Science 378, eaba1624.
June C et al. (2018). CAR T cell immunotherapy for human cancer. Science 359, 1361-1365.
Larson R and Maus M. (2021). Recent advances and discoveries in the mechanisms and functions of CAR T cells. Nat Rev Cancer 21, 145-161.
Li H et al. (2022). Multidimensional control of therapeutic human cell function with synthetic gene circuits. Science 378, 1227-1234.
Sterner R and Sterner R. (2021). CAR-T cell therapy: current limitations and potential strategies. Blood Cancer J 11, 69.
You may also be interested in...

View more Immunology or Guest Blog blogs















